I have written recently about WHO’s 75th anniversary and key historic accomplishments during its lifetime such as the eradication of smallpox (1980), framework convention on tobacco control (2003), and revision of the international health regulations (2005). This list should also include the Declaration of Alma Ata (1978) which identified primary health care as central to health for all.
However, the trick to understanding WHO’s impact is not only the milestone accomplishments like those above, but the many things WHO does day in and day out, country by country, to achieve major public health benefits.
The quintessence of WHO’s strategy can be described in four words: measurable impact in countries. Turning strategy into actual results (and being able to succinctly describe them) is the core function of any organization.
If you’re looking for evidence that WHO has become more results-focused over the past six years under Dr Tedros’ leadership, you need to look no further than his speech at the 76th World Health Assembly. It laid out progress on the SDG-based triple billion targets, described 10 highlighted accomplishments, and invited Member States to work with the WHO Secretariat to identify ways to speed up SDGs.
During the Assembly, WHO launched its World Health Data Hub (an incredible new resource you should check out and bookmark!) and annual results report for 2022 (see here for all of them). This post describes those results.
Triple Billion targets are lagging
In an earlier post I described the SDG-based triple billion targets, which are primarily the responsibility of countries. Unfortunately, the world is off track to reach most of the triple billion targets and the health-related SDGs. Urgent action is needed to accelerate progress, or the world may fall further off track. Here is the progress on the triple billion:
The Results Report details progress on these targets; I have extracted the relevant text below:
The indicators for healthier populations are influenced by multisectoral policy actions to address determinants of health. Substantial progress has been made, and the current trajectory indicates that this target will likely be met by 2025; however this will be insufficient progress to be on track to reach the related SDGs by 2030. For example, the global age-standardized prevalence of tobacco use remains high. The prevalence of adult obesity continues to be on the rise in all WHO regions, with no immediate sign of reversal. Air pollution has not been tackled in many areas of the world. Data from the pandemic period continue to be sparse, so the full extent of the impact of the COVID-19 pandemic on various health determinants and policies is not yet quantified.
The world is off track to meet the Universal Health Coverage (UHC) billion target by 2025 and related SDGs by 2030. The disruptions caused by the COVID-19 pandemic have had a significant impact on many indicators, only some of which are recovering. Overall measures of progress are largely driven by increased HIV service coverage. Service coverage for routine childhood vaccination, malaria, tuberculosis, noncommunicable and other diseases and preventive services all continue to lag, while indicators for financial hardship have worsened.
Progress in health emergencies protection is not on track to reach the billion target by 2025. Improvement in preparedness, measured through core capacities related to the International Health Regulations (2005) and reflected by the Prepare indicator, contributed positively in 2022. However, pandemic-related disruptions to high-priority pathogen vaccination programmes, measured under the Prevent indicator, need to be resolved. Efforts are continuing in order to assess the best way to measure health emergencies protection, including the integration of timeliness targets for detection, notification and response to health emergencies.
After more than three years of the COVID-19 pandemic, the world concurrently faces crises from climate change and natural disasters, conflicts, continuing erosion of human rights, and a tightening macroeconomic environment with increased inflation and cost of living, increasing public debt and reduced fiscal space, and challenging energy and food crises. All these risks have a direct bearing on health and wellbeing and urgent action is needed to get on track towards UHC, the SDGs, and Health for All.
Highlighted achievements
WHO (or to be precise, the WHO Secretariat) aims to support countries to reach the triple billion targets and health-related SDGs. Here are the 10 highlighted achievements of WHO, organized using WHO’s 5P strategy, with text taken directly from the Results Report.
Promote
More than 133 countries increased or introduced a new health tax between 2017 and 2022, showing that Member States are increasingly equipped to use fiscal measures to improve health, reduce health care costs and generate a revenue stream for development – owing in part to increased technical support and updated guidance from the Secretariat. Now 146 countries are protected by at least one measure of the MPOWER technical package; 60 countries are on track to achieving the global targets for reducing tobacco use; and health taxes are part of a comprehensive strategy for preventing noncommunicable diseases, which kill 41 million people every year.
Ground-breaking international targets were set in order to address the use of antimicrobial agents across the animal, farming and human health sectors, and thereby tackle the devastating health and economic impacts of antimicrobial resistance – 1.3 million deaths were attributable to antimicrobial resistance in 2019. The Secretariat supported the development of targets for 2030 by advocating with governments and serving as secretariat for the Quadripartite, which includes the Food and Agriculture Organization of the United Nations, World Health Organization, World Organization for Animal Health and United Nations Environment Programme. (This could also fit under “provide.”)
Provide
In 2022, the first-ever all-oral treatment regimens for multidrug-resistant tuberculosis were made available. The Secretariat developed and introduced guidelines recommending the use of the new, all-oral treatment of multidrug-resistant tuberculosis, thereby contributing to its uptake in 109 countries. A reduction in treatment time from 18 months to 6 months significantly improves the quality of life for people with multidrug- and rifampicin-resistant tuberculosis.
The world’s first malaria vaccine, RTS,S/AS01, has been administered to 1.2 million children in Ghana, Kenya and Malawi through continuing pilot programmes, resulting in a substantial drop (an estimated 30%) in admissions of children with severe malaria to hospital and an important decline in child deaths (a 10% fall in all-cause mortality among children who are of suitable age to receive the vaccine). WHO issued prequalification approval for the RTS,S /AS01 vaccine and is the scientific lead and coordinator of the malaria vaccine implementation programme; an estimated one life is saved for every 200 children so vaccinated.
The 2022 rounded estimates indicate a reduction in the global health workforce shortage to 15 million in 2020 and a projected global shortage of 10 million in 2030 based on current trends (mostly depicting a pre-COVID-19 situation). This is a significant decrease as compared with the earlier projection of a shortage of 18 million by 2030. However, the African and Eastern Mediterranean regions show less progress, will bear an increasing share of the total shortage in 2030 and may need to review their health labour market policies and investments.
Protect
A fund dedicated to pandemic preparedness and prevention, the Pandemic Fund, was created with the financing needs and gap validated by G20 finance and health ministers. WHO hosted the secretariat of the G20 Joint Finance and Health Task Force, and contributed expertise on financing pandemic preparedness and prevention. The Pandemic Fund has an initial budget of US$ 1.6 billion and the WHO-chaired technical advisory panel will make key inputs into the scope of work funded. The Task Force has been extended into a multiyear arrangement.
The Contingency Fund for Emergencies released funding, in as little as 24 hours, to 70 graded emergencies in 2022, in line with WHO’s Emergency Response Framework. The Secretariat conducted 65 rapid risk assessment for 53 events in 30 countries, as well as 14 assessments for multicounty events. A highlight was the completion and circulation of 21 rapid risk assessment reports within a single week. Risk at the national level was assessed as very high or high for 90% of those events, which were mainly caused by cholera, measles, monkeypox/mpox, COVID-19, dengue, Ebola virus disease, Lassa fever and undiagnosed diseases. In total US$ 87.77 million were released to fund the initial response to acute events and scale up life-saving health operations in protracted crises in response to escalating needs.
More than 50 countries transitioned crucial infrastructure from reliance on resources from the Global Polio Eradication Initiative, integrating their polio assets, tools and knowledge to sustain critical functions related to immunization, disease surveillance and emergency response. The 37 countries that have completed the transition in the African Region remain polio-free. Polio networks, which in the Eastern Mediterranean Region have been repurposed to reach high-risk and hard-to reach populations with a broader package of health services, have responded to public health emergencies, such as outbreaks of cholera. In the South-East Asia Region, the integrated surveillance and immunization networks in the five priority countries were geared towards reversing the impact that the COVID-19 pandemic has had on essential immunization, as the region hosts around 35% of the world’s “zero-dose children”. WHO’s funding commitment of US$ 33.2 million from the Core Voluntary Contributions Account has been catalytic to sustaining the essential polio functions through integration and ensuring their long-term sustainability.
Power
The mRNA hub in South Africa was established to build vaccine production capacity and enhance outbreak response in low- or middle-income countries. In 2022, the hub’s manufacturing process was developed, and mRNA technology started to be transferred from the hub to 15 spokes across all WHO regions. A training hub in the Republic of Korea was set up and has trained 300 staff in low- or middle-income countries on biomanufacturing and undertaking research on alternative uses for medical countermeasures. The model is being explored for applications to other medical technology needs.
WHO reported an estimated 14.9 million excess deaths globally in 2020–2021 as a result of the COVID-19 pandemic – reversing years of improvement in population health in many countries around the world. The effort to assess the true toll of the COVID-19 pandemic on population health at country, regional and global levels was joined by other United Nations entities and leading scientists worldwide, who consulted extensively with Member States using an effective online country portal supported by the World Health Data Hub. An update on both the magnitude and age/sex distribution of the excess mortality is ongoing and is expected to bring more clarity to the impacts of the pandemic on the triple billion targets and the health-related targets of the Sustainable Development Goals.
These achievements are drawn from a much longer list covered in the results report, which also systematically measures outputs using a score card approach. What do you think of these achievements?
WHO Results Framework
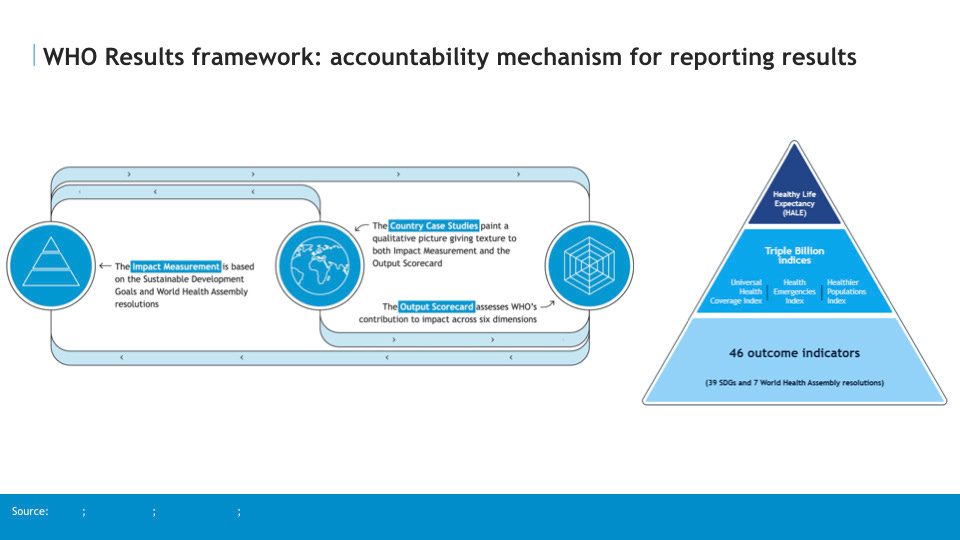
Underlying the reporting of results is WHO’s results framework, which combines measurement of impact (comprised of healthy life expectancy, triple billion indices, and outcome indicators largely based on SDGs), outputs (measured using an output scorecard based on the strategic shifts of leadership, global goods and country support plus gender, equity and rights, value for money, and leading indicators), and country case studies (to connect these outputs and outcomes in context).
Conclusion
The essence of WHO’s ten-year strategy under Dr Tedros can be described in just four words: measurable impact in countries. This post has described WHO’s results at the midpoint of this 10 years and shows that much progress has been made in transforming WHO into an organization tightly focused on results. At the same time, many lessons have been learned about how to further close the gap between strategy and implementation for a more results-based WHO. These lessons are applicable to any organization seeking to become more results-based, and they will be the focus of my next post.





Valuable report Peter.
You outline how trends in NCDs are off track. And recommend more attention to old policies that are in my view too unwieldy, too many to focus governments scarce resources, and fail to engage all stakeholders with expertise, scale and capabilities to compliment WHO and government.
A few efforts WHO could drive that would materially impact the lives of billions:
Global long term well designed campaigns to tackle stigma and mental illness. That unblocks deep discrimination against mental health by physicians, media, and employers.
Global long term support for physical activity-that would tackle many NCDs and mental health. It triggers many positive health behaviors.
Global strong support for tobacco harm reduction as opposed to current opposition. That could open the doors to governments and industry to reduce 1 billion smokers. It could save 3 million premature deaths annually from 2030-2060.
Thank for allowing us to get key insights about the latest WHO report in a very concise manner.
One aspect that is of concern in my practice is how we can ensure the results achieved themselves remain sustainable across time.